DH turned 65 at the end of last year. He recently got into the VA system but we thought he should also to get a Medicare primary care physician. He has the AARP United Healthcare Advantage plan. He sees the chiro a couple of times a year but hasn't seen a doctor in years.
He had a full physical at the VA and everything was good except his total cholesterol is high (and always has been) at 260. His LDL is 174 and his HDL runs around 60. He has never smoked, has been the same normal weight for at least the last 20 years, is active and is a glass half-full personality. His mother lived a healthy life to nearly 95 (with elevated cholesterol). His father lived to his mid-70's but seriously abused his body with smoking (1.5 lungs removed), drinking (lifelong alcoholic), and anger.
When the VA saw his numbers, his lifestyle, and his family history, they were curious about what might be going on inside and suggested he might want to do a scan to determine a calcium score (I think). Nobody suggested he start taking a statin.
When he went to see his Medicare PCP (a guy about 40), his first comment was about DH's high LDL and how risky it was. DH let his PCP know he wasn't going to be taking a statin. I let PCP know we had an NMR study we had done through the internet and wondered whether he could interpret the results. He said he could not but there was an Internist a couple doors down who was a total cholesterol nerd and could read it.
DH and I went to see the Internist and, based on the NMR test, the Internist gave us some interesting information about my husband's situation. DH has high LDL-C and very high LDL-P (quantity of particles). The internist assumed that DH's system would show markers of inflammation and he would need to take a statin (which wasn't going to happen). He said he had this whopper test DH could take that would give much more info than just the regular stuff and tell him whether his system was inflamed (which would definitely put him at cardiovascular risk).
We discussed DH watching (okay, me watching!) what he ate for the next 8 weeks and whether we should do a baseline test and one after 8 weeks or just one after 8 weeks. I requested we do a baseline test so DH would know where he was starting.
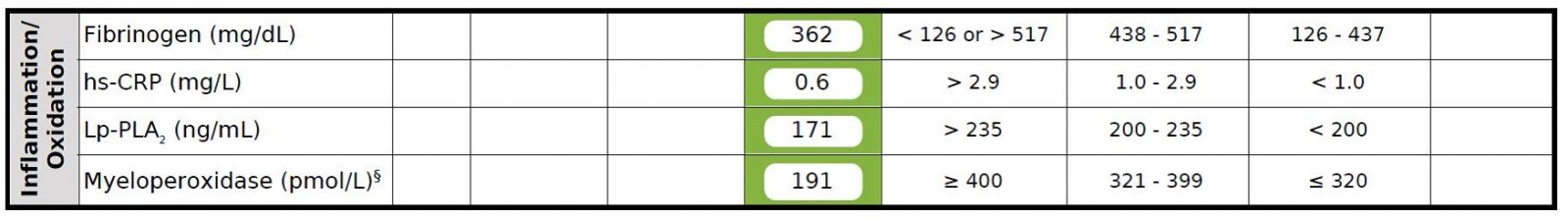
We received the result of the baseline test and DH's system shows no, none, nada, zero indication of inflammation. DH is solidly in the green on all the inflammation markers. This is before DH did anything related to his diet (which really isn't bad to start with). We have a follow-up appointment in early May but when we picked up the test from his office, the nurse said the doctor's only recommendation was for DH to take some fish oil because his DHA + EPA level was low. No mention of a statin. Based on the nurses other comments, it seems the Internist is no longer concerned about DH cardiovascular risk. We'll find out more in May. IMO, I think the Internest was surprised by the total lack of inflammation even though LDL-C and LDL-P were both elevated.
If you ever want to do a cardiovascular risk assessment beyond your HDL and LDL, this test is pretty interesting. There are 6 pages of results and 2 pages of explanation. About 50 different things are measured. You can get more info on the test at the myHDL website. The test doesn't really have a name. The header just says 'Laboratory Results.' I guess it's just 'the' test.
He had a full physical at the VA and everything was good except his total cholesterol is high (and always has been) at 260. His LDL is 174 and his HDL runs around 60. He has never smoked, has been the same normal weight for at least the last 20 years, is active and is a glass half-full personality. His mother lived a healthy life to nearly 95 (with elevated cholesterol). His father lived to his mid-70's but seriously abused his body with smoking (1.5 lungs removed), drinking (lifelong alcoholic), and anger.
When the VA saw his numbers, his lifestyle, and his family history, they were curious about what might be going on inside and suggested he might want to do a scan to determine a calcium score (I think). Nobody suggested he start taking a statin.
When he went to see his Medicare PCP (a guy about 40), his first comment was about DH's high LDL and how risky it was. DH let his PCP know he wasn't going to be taking a statin. I let PCP know we had an NMR study we had done through the internet and wondered whether he could interpret the results. He said he could not but there was an Internist a couple doors down who was a total cholesterol nerd and could read it.
DH and I went to see the Internist and, based on the NMR test, the Internist gave us some interesting information about my husband's situation. DH has high LDL-C and very high LDL-P (quantity of particles). The internist assumed that DH's system would show markers of inflammation and he would need to take a statin (which wasn't going to happen). He said he had this whopper test DH could take that would give much more info than just the regular stuff and tell him whether his system was inflamed (which would definitely put him at cardiovascular risk).
We discussed DH watching (okay, me watching!) what he ate for the next 8 weeks and whether we should do a baseline test and one after 8 weeks or just one after 8 weeks. I requested we do a baseline test so DH would know where he was starting.
We received the result of the baseline test and DH's system shows no, none, nada, zero indication of inflammation. DH is solidly in the green on all the inflammation markers. This is before DH did anything related to his diet (which really isn't bad to start with). We have a follow-up appointment in early May but when we picked up the test from his office, the nurse said the doctor's only recommendation was for DH to take some fish oil because his DHA + EPA level was low. No mention of a statin. Based on the nurses other comments, it seems the Internist is no longer concerned about DH cardiovascular risk. We'll find out more in May. IMO, I think the Internest was surprised by the total lack of inflammation even though LDL-C and LDL-P were both elevated.
If you ever want to do a cardiovascular risk assessment beyond your HDL and LDL, this test is pretty interesting. There are 6 pages of results and 2 pages of explanation. About 50 different things are measured. You can get more info on the test at the myHDL website. The test doesn't really have a name. The header just says 'Laboratory Results.' I guess it's just 'the' test.