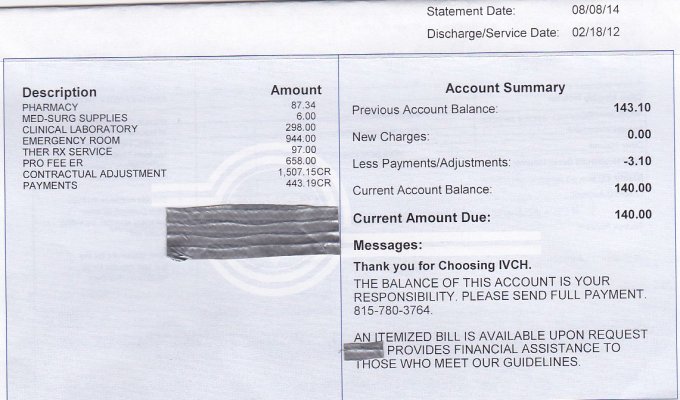
On Feb 8, 2012, I went to the emergency room in our local hospital for a worrisome injury to my elbow. Yesterday, I received a bill (see below) for $140.
The treatment was covered by Medicare, and my supplemental insurance policy. Since the incident occurred over two and a half years ago, I no longer have a copy of the original billing, but am positive that we received no outstanding bill in the months after the accident. Having been embroiled in a hospital billing dispute over 25 years ago... along with a threat to my credit standing, we no longer let any overdue bill stand, knowing what can happen when a bill has been turned over for collection.
So, here are the questions:
1. For what period of time can the billing department require payment, even though there have been no interim bills.
2. How long should we have to keep copies of billing?
3. Should I choose not to pay, how can I challenge the bill, to avoid having it show up on my credit report?
4. If I should need emergency services in the future, can the hospital refuse treatment?
5. If my doctor is affiliated with the hospital, and I require hospitalization for non-emergency services, can the hospital refuse to accept me as a patient?
6. In this, and many cases where we go to a business for services, there is usually a paper that we have to sign, agreeing to submit to binding arbitration for any disputes. I have understood that the cost of this arbitration may go into many thousands of dollars. Certainly not worth it for low value dollar amounts such as this.
7. Can I require a record of previous billings for the same admission.
In the past, dealing with the same hospital, and receiving a bill before our supplemental insurance claim was received by the hospital... (two months), I questioned the billing office as to the length of time before they would turn the bill over for collection. In that case, a tough talking billing manager told me that it was their business, and their choice.
While I am reasonably sure that I will pay the bill... simply to avoid the angst, I feel that I have no choice... no alternative. At the same time, I worry that something like this could happen in the future, where the amount could be more, and any binding arbitration could go against me and in favor of the battery of lawyers that the hospital maintains.
Could this happen to you? What would you do?
The treatment was covered by Medicare, and my supplemental insurance policy. Since the incident occurred over two and a half years ago, I no longer have a copy of the original billing, but am positive that we received no outstanding bill in the months after the accident. Having been embroiled in a hospital billing dispute over 25 years ago... along with a threat to my credit standing, we no longer let any overdue bill stand, knowing what can happen when a bill has been turned over for collection.
So, here are the questions:
1. For what period of time can the billing department require payment, even though there have been no interim bills.
2. How long should we have to keep copies of billing?
3. Should I choose not to pay, how can I challenge the bill, to avoid having it show up on my credit report?
4. If I should need emergency services in the future, can the hospital refuse treatment?
5. If my doctor is affiliated with the hospital, and I require hospitalization for non-emergency services, can the hospital refuse to accept me as a patient?
6. In this, and many cases where we go to a business for services, there is usually a paper that we have to sign, agreeing to submit to binding arbitration for any disputes. I have understood that the cost of this arbitration may go into many thousands of dollars. Certainly not worth it for low value dollar amounts such as this.
7. Can I require a record of previous billings for the same admission.
In the past, dealing with the same hospital, and receiving a bill before our supplemental insurance claim was received by the hospital... (two months), I questioned the billing office as to the length of time before they would turn the bill over for collection. In that case, a tough talking billing manager told me that it was their business, and their choice.
While I am reasonably sure that I will pay the bill... simply to avoid the angst, I feel that I have no choice... no alternative. At the same time, I worry that something like this could happen in the future, where the amount could be more, and any binding arbitration could go against me and in favor of the battery of lawyers that the hospital maintains.
Could this happen to you? What would you do?
Attachments
Last edited: